WE ARE A TEAM DEVOTED TO EXCELLENCE
in the art and discipline of cosmetic and reconstructive eyelid and facial surgery
COSMETICS
RECONSTRUCTIVE
Eyelid
Eyelashes Disease
Read More
Eyelashes Disease
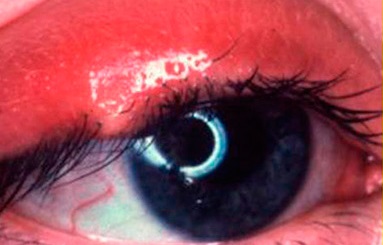
Disorders of the eyelashes may cause eye redness, tearing, constant irritation, foreign body sensation, and sensitivity to light and wind to name a few symptoms. If the condition is not treated properly and promptly, patients may present with recurrent eye infections and even eye ulcers that can compromise vision. Two conditions that produce these symptoms are:
Trichiasis: is a condition in which the eyelashes grow or rotate toward the eyeball. Producing these continuous friction against the eye surface (conjunctiva and cornea)
Distichiasis: is a condition in which there is abnormal growth of row (s) extra on the lid margin to the eyeball. Producing these tabs continuous friction against the eye surface (conjunctiva and cornea)
Both Distichiasis Trichiasis as the cause redness and eye irritation, tearing continuous sensitivity to light and wind. If not treated promptly and properly, the patient’s vision may be compromised. There are minimally invasive treatments such as radio-frequency for simple cases to surgery for complex cases

Corrective Plastic Surgery
Read MoreEyelid Reconstruction/ Corrective Plastic Surgery
Defects in the eyelid may result from a variety of situations, most commonly after trauma or tumor excision, and specialized eyelid reconstruction is mandatory. Simple superficial defects in the eyelid may occur after minor trauma or removal of small growths. Many of these require nothing more than local wound care and will heal on their own in a week to 10 days. Some simple superficial defects may require a few sutures with the same local wound care. After traumatic injuries or removal of larger growths or skin cancers, larger defects may extend through the entire lid. Many of these can be sutured together directly, but many others may require more complex reconstructions. In these more complex cases, the surgeon will need to use transfer of adjacent tissues (what we call “flaps”), or transfer of skin from other parts of the eyelid, face, or body (what we call “skin grafts”) to complete the reconstruction. Some of these more complex reconstructions may require more than one operation to complete (know as “staged reconstruction”). Another important group of patients who might need eyelid reconstruction are patients who had a surgical procedure performed elsewhere that did not realize their initial goals. Many patients come to Dr. Lin Yang for corrective plastic surgery or “Touch-ups.” This can be caused by a variety of factors such as: complications due to scarring, outdated procedures or just poor technique.
Blepharospasm
Read More
Blepharospasm
Essential blepharospasm is an idiopathic disorder characterized by involuntary spasm of the eyelids and sometimes other facial muscles. Most patients also have dry, irritated eyes and in most patients, symptoms are worse when exposed to sunlight or bright lights indoors.
Botox injections are the initial treatment. Some patients’ symptoms cannot be controlled with Botox alone. For this group of patients, Myectomy surgery is next line of treatment for them. You can consult Dr. Lin Yang for further details regarding Myectomy surgery.
Eyelid Cancer
Read More
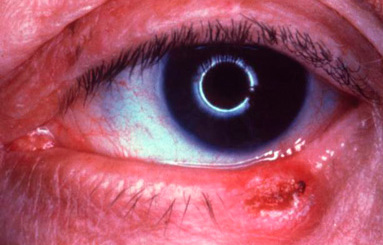
Eyelid Cancer
The face and eyelids are very common locations for skin cancer. Many times skin cancers may appear as benign growths. Other times they can develop cancerous characteristics over a relatively short time. Potential warning signs are new growths with elevated, irregular boarders, coloration, indentation, or ulceration, along with bleeding, crusting, and/or distortion of the normal skin structure. If skin cancer forms along the edge of the eyelid it often causes the eyelashes to fall out. Excessive sunlight is the single most important factor associated with skin cancers on the face, though skin cancers may also be hereditary.
There are two very important principles in the treatment of eyelid skin cancers-complete removal and reconstruction. Complete removal of the tumor is critical to minimize the possibility of recurrence. Once the tumor has been completely removed, reconstructive surgery is performed to make a new eyelid or repair the defect. The area of concern is first biopsied to determine if it is in fact a cancer. If the biopsy is not cancerous, no further treatment is required. If the biopsy is cancerous, most cancers are then removed using the MOHS technique because this method has the highest cure rate and preserves the most normal tissue around the eyelids and face.
Eyelid Malposition
Read More
Eyelid Malposition
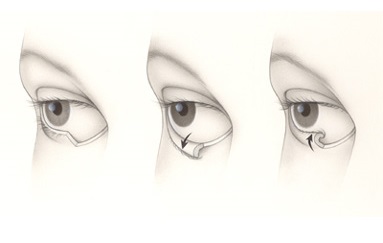
The eyelids are essential for the protection of the eyes. Abnormalities of contour, strength, or position can dramatically affect ocular comfort and more importantly our vision. Two typical eyelid malposition problems are entropion and ectropion.
Entropion is the “in” turning of the lower eyelid. Entropion occurs most commonly as result of aging. Infection and scarring inside the eyelid are other causes of entropion. When the eyelid turns “inward,” the eyelashes and skin rub against the eye, making it red, irritated, watery and sensitive to light and wind. If entropion is not treated, an infection or ulcer may develop on the cornea (the clear surface of the eye). With surgery, the eyelid can be turned to its normal position, protecting the eye and improving the symptoms.
Ectropion is the “out” turning of the lower eyelid. Patients with ectropion have a sagging lower eyelid that leaves the eye exposed and dry. It is caused by a lack of tone of the delicate muscles that hold the lid taut against the eye. Excessive tearing is common with ectropion, but wiping the tears away only causes the lid to sag more. Ectropion is most common among people over the age of 60. The irritation can be temporarily relieved with artificial tears and ointments to lubricate the eye; however surgery to tighten the lid is usually necessary to correct this problem.

Ptosis (Droopy Eyelids)
Read More
Ptosis (Droopy Eyelids)
Ptosis (pronounced toe’ sis), or drooping of the upper eyelid, may occur for several reasons such as: disease, injury, birth defect, previous eye surgery, eyelid rubbing, eyelid manipulation from contact lens use, and age.
Usually ptosis is caused by a weakness of the levator muscle (muscle that raises the lid), a partial detachment of the muscle from the skeleton of the eyelid (the tarsus), or a problem with the nerve that sends messages to the muscle. Patients often have difficulty blinking, which may lead to irritation, infection and eyestrain. Chronic attempts to keep the droopy eyelid open can actually result in a “dry eye” problem.
Ptosis does not usually improve with time, and nearly always requires corrective surgery. In most cases, surgery is performed to strengthen or tighten the levator muscle and lift the eyelid. If the levator muscle is especially weak, the lid and eyebrow may be lifted. Ptosis surgery and upper eyelid blepharoplasty surgery are the most common reconstructive surgeries performed by Dr. Lin Yang. Lifting of a droopy eyelid is achieved thru an incision of less than an inch and it is often well concealed within the normal eyelid crease. Generally, this procedure is performed in conjunction with upper eyelid blepharoplasty.
Correction of one or both droopy upper eyelids may improve a “sleepy-eyed” appearance, enhance the field of vision, increase light entering the eye and improve overall visual acuity, ameliorate dry eye symptoms in some individuals, and resolve end-of-day “tension” headaches and neck aches in people who chronically raise their eyebrows to see throughout the day.
Tear Duct

Dry Eyes
Read More
Dry Eyes
Dry Eyes or Keratitis Sicca is a major cause of tearing. Many times, it is under-diagnosed. Often the patients complain of foreign body sensation associated with redness and watery eyes. Depending on the degree of the dryness of the eye, the treatment starts with artificial tears for mild to moderate dry eye patients.
For the severe dry eye patients, treatment option could vary from non surgical placement of tear duct plugs to surgical tear duct occlusion to retain more tear.

Tear Duct Trauma
Read MoreTear Duct Trauma
An important group of facial traumas involve the eyelid; more importantly, within this group of eyelid traumas, the tear duct system can be damaged during these traumas. If not properly diagnosed and treated, the patient can have permanent tearing. Dr. Lin Yang is specializes in treating these types of traumas.
Tear Duct Disease
Read MoreTear Duct Disease
Tears are made primarily by the lacrimal gland, wich is located in the upper inside corner of the upper eyelid. With each blink, tears are carried from the eye surface thru the lacrimal puncta to the lacrimal canaliculi and then to the lacrimal sac down to the nasolacrimal duct into the nose. Different problems along this trajectory can cause blockage of the tear duct system. These include blockage of the external tear drain (punctal stenosis), blockage of the portion of the tear drain in the eyelid (canalicular stenosis) and blockage of the tear drain in the nose (nasolacrimal duct obstruction). Tearing is fairly common and when it improves with the use of artificial tears or only happens on rare occasions, it requires no further treatment. However, blockage of the tear drainage system externally, in the eyelid, or in the nose can require surgical correction. Dr. Lin Yang is an expert in diagnosing and surgically managing abnormalities of the tear drainage system.Orbit

Orbital Trauma
Read More
Orbital Trauma
The bones in and around the eye socket are often fractured when there is trauma to the face. The most common causes of fracture are assault, motor vehicle accident, and recreation related accidents.
These fractures can impact both form and function. If the fracture is adjacent to one of the eye muscles, such as in a blow out fracture of the orbit, it may cause double vision. Fractures of the jaw or bones adjacent to the muscles that move the jaw can cause problems chewing.
Fractures of the facial bones can also cause deformities of the face, such as a sunken looking eye or a flat cheek bone. All these fractures require surgery and have more favorable outcomes when operated soon after the injury.

Orbital Tumor
Read More
Orbital Tumor
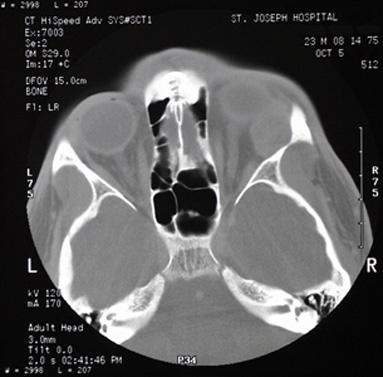
The orbital socket containing the eye socket or the eyeball, extraocular muscles, nerves and vessels of the eyeball. Some tumors can form in this space or migrate to this area from other parts of the body.
It is important that the patient undergo a thorough eye examination and additional imaging studies such a CT scan.

Thyroid Eye Disease
Read More
Thyroid Eye Disease
Thyroid Eye Disease or Grave’s Eye Disease is perhaps the most common orbital disease in our population. It is an autoimmune problem, most commonly noted in patient with a history of either high or low thyroid hormones. However, some patients might demonstrate no evidence of thyroid dysfunction. Thyroid Eye Disease can go into periods of remission as well. When it has been inactive for a period of more than 6 months, it’s less likely to recur.
Thyroid Eye Disease can be divided in stages. During the early part of the disease, the eyes become red, swollen, and watery. This early part of the disease is referred to as the active and inflammatory phase of the disease. During this initial phase of the disease, patients may benefit from treatments to reduce inflammation such as anti-inflammatory medications or injections, topical lubricating eye drops and ointments, and in some cases, referral for orbital radiation. In the later part of the disease the eyes may bulge out of the socket, the eyelids may be open too wide, or the patient may have double vision. In this small percentage of patients, orbital decompression may be called. Symptoms for these patients may include:
- Pain in the eyes when looking up, down, or sideways
- Dryness, itching, dry eyes, difficulty wearing contact lenses
- Inflammation and swelling of the eye, and its surrounding tissues
- Swelling in the orbital tissues which can cause sufferers to have a wide-eyed or bulging stare

Dr. Chun Cheng Lin Yang
Dr. Lin Yang specializes in cosmetic and reconstructive surgery of the eyelids, tear drainage system and the orbits (Oculoplastics, Lacrimal, and Orbital Surgery). He is the first ophthalmologist (eye MD) in Costa Rica with formal fellowship training at a premier oculoplastics & orbital surgery program in the United States. After returning to Costa Rica, he pioneered the recognition and accreditation of Oculoplastics, Lacrimal and Orbital Surgery by the Costa Rican College of Physicians and Surgeons. Dr. Lin Yang is the first Costa Rican and Central American oculoplastics and orbital specialist inducted to the American Society of Ophthalmic Plastics and Reconstructive Surgery (ASOPRS).
BOARD CERTIFIED IN:
>> Ophthalmology
>> Ophthalmic Plastics & Reconstructive and Orbital Surgery
EDUCATION:
BA (Chemistry)
>> Baylor University
MD
>> Universidad Autonoma de Centro America
MSc
>> Universidad de San Carlos de Guatemala
RESIDENCY & FELLOWSHIPS:
>> Unidad Nacional de Oftalmologia
Universidad de San Carlos de Guatemala
>> Center for Facial Appearances, Utah, USA
CREDENTIALS:
>> American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS)
>> American Academy of Ophthalmology (AAO)
>> Pan-American Association of Ophthalmology (PAAO)
>> Sociedad Centroamericana de Oculoplastica y Orbita
>> Colegio de Medicos y Cirujanos de Costa Rica
>> Colegio de Medicos y Cirujanos de Guatemala
HONORS:
>> Gillingham Pan-American Fellowship
>> International Council of Ophthalmology Fellowship




















